Health & sanitary info
Vaccines
Yellow fever is the only immunisation required, but some more are advisable
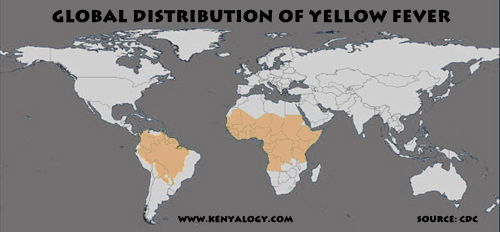 For visitors to Kenya, the only obligatory vaccine is yellow fever (not required for babies younger than 1 year old), but it is mandatory only for travellers coming from high risk areas, which roughly include the whole middle strip of Africa from the Sub-Saharan line down to Angola-Congo-Tanzania, and South America south of the Panama Canal except the Southern Cone (see map).
For visitors to Kenya, the only obligatory vaccine is yellow fever (not required for babies younger than 1 year old), but it is mandatory only for travellers coming from high risk areas, which roughly include the whole middle strip of Africa from the Sub-Saharan line down to Angola-Congo-Tanzania, and South America south of the Panama Canal except the Southern Cone (see map).
Mind you, in one occasion I was requested to show my yellow fever vaccine certificate to an unfriendly Kenyan immigration officer, even though I had just landed in Nairobi from Europe.
One important note: regardless of legal requirements, getting the jab is highly advisable, since in Kenya you can actually catch yellow fever. Coming from a non-infected country will not protect you against the disease if the carrier mosquito bites you (those poor little bugs don't know you're American or European).
Beyond this, most countries' travel health services recommend vaccinations against tetanus, diphtheria, typhus, poliomyelitis, hepatitis A and B. Meningococcal meningitis and cholera may be added for those at risk, e.g. workers in slums or refugee camps.
Even though HIV prevalence rate has declined in recent years, following governmental campaigns promoting safe sex, AIDS is still pretty much widespread, particularly among sex workers. Take precautions if you engage in sexual relationships.
For all matters concerning vaccinations and other health issues, always follow the advice by your national travel health service. Be sure to consult 6 to 8 weeks ahead of your trip.
Malaria & mosquitoes
Do your best to prevent bites and take your malaria pills
Paludism or malaria is a severe disease communicated by the bite of the 'Anopheles' mosquito carrying any of four species of the 'Plasmodium' parasite. 'Plasmodium falciparum', the most prevalent type in Africa, is also the deadliest. There is no vaccine yet.
The World Health Organization (WHO) estimates that half of the world's population lives in risk areas, which span 99 countries. Sub-Saharan Africa is the most affected region. Every minute a child dies in Africa from malaria. In all the world, between half a million and one million people died from the disease in 2010.
Enough reasons to be concerned, but not obsessed. If you are only travelling to Nairobi or to the highlands above 2,500 m (8,200 ft), your risk is between low and none. Otherwise, if you visit any game park, you are at risk (see map below).

The WHO publishes the following ABCD of malaria protection for travellers:
A. Be aware of the risk, the incubation period and the main symptoms.
B. Avoid being bitten by mosquitoes, especially between dusk and dawn.
C. Take antimalarial drugs (chemoprophylaxis) to suppress infection where appropriate.
D. Immediately seek diagnosis and treatment if a fever develops one week or more after entering an area where there is a malaria risk, and up to 3 months after departure.
Concerning chemoprophylaxis, recommendations may vary slightly among different countries' travel health authorities, but there is a general agreement that chloroquine (Nivaquine™, Resochin™, Aralen™) is not sufficient as a chemoprophylactic against malaria for travellers to Kenya, since chloroquine resistance is widespread. Even taking chloroquine together with other drugs such as proguanil (Paludrine™), or the combination of both (Savarine™), is not considered safe.
The most usually prescribed malaria tablets for travellers to Kenya are atovaquone/proguanil (Malarone™) or doxycycline (available generically) or mefloquine (Lariam™). Lariam has been reported to produce neurological and psychiatric disorders in sensitive patients or with previous symptoms. If you take Lariam, start at the very least two or three weeks before your trip, hence you will be able to check at home if you suffer from any secondary effects. Prophylaxis must always be continued until four weeks after returning from the risk area. Consult with your national travel health service to know which is the most suitable medication for you.
 In addition to antipaludic chemoprophylaxis, it is advisable to add some protection against mosquito bites between dusk and dawn. Wear long pants and sleeves and use a mosquito repellent containing 35-50% of N,N-diethyl-m-tholuamide (DEET), which for more than 50 years has been the preferred choice. DEET-based repellents should be reapplied every 4-6 hours. Both the United States Centers for Disease Control and Prevention (CDC) and the UK's National Travel Health Network and Centre (NaTHNaC) consider that DEET is safe for babies older than two months and for pregnant and breastfeeding women. Still, some manufacturers may recommend more restrictions for use.
In addition to antipaludic chemoprophylaxis, it is advisable to add some protection against mosquito bites between dusk and dawn. Wear long pants and sleeves and use a mosquito repellent containing 35-50% of N,N-diethyl-m-tholuamide (DEET), which for more than 50 years has been the preferred choice. DEET-based repellents should be reapplied every 4-6 hours. Both the United States Centers for Disease Control and Prevention (CDC) and the UK's National Travel Health Network and Centre (NaTHNaC) consider that DEET is safe for babies older than two months and for pregnant and breastfeeding women. Still, some manufacturers may recommend more restrictions for use.
Okay, DEET is sticky and smells nasty, it will melt plastic and make you feel everything you eat smells of DEET. Not very nice, but highly effective.
Other non-DEET repellents are based on dimethylphthalate (DMP), which must be used at a concentration of at least 40%. For children under 10 years and over 30 months, it is advisable to use repellents based on ethylhexanediol (EHD). This substance, specially effective against 'Anopheles', must be used at a concentration of 30-50%. Other repelling compound is N-buthyl-N-acetyl-3-ethylaminepropionate (better known as 35/35), which is used at 20-30%. Other repellents proved effective are Mosiguard™ (lemon eucalyptus extract, not recommended for children under 3 years) and Autan™ (Icaridin/Picaridin/Bayrepel). Repellents may be found as a lotion, cream, spray or stick. Whatever repellent you choose, follow the manufacturer's instructions.
One more word on repellents. In certain locations in Kenya and at certain times of the year, other bugs can be a greater nuisance than mosquitoes, e.g. tsetse flies in Meru National Park. Check that your bug repellent is also effective against these nasty critters. Even regular flies can be a pain in the neck in some places.
And yet one last word about repellents. Do not trust on electronic devices (e.g. ultrasonic repellers) which claim to be effective against mosquitoes. There is no scientific evidence supporting such claims, and they are considered by many as completely useless.
For added safety, bed mosquito nets are available at most lodges. They can be impregnated with insecticides like pyrethrine derivatives (permethrine or deltamethrine). You can also use spray or electric insecticides, which are provided at some lodges. If you bring your own electric insecticide, check with the lodge staff for the hours at which there is power supply, since lodges that are disconnected from the power grid use their own generators and may switch them off during daylight hours and through the night. Battery-operated electric insecticides can be a good replacement, specially if you go camping.
Med insurance
Be sure to be covered // The Flying Doctors Service is a good choice
You should get some medical insurance to cover the expenses for ambulance transport, hospitalisation and travelling back home. If you travel on a package tour, you will possibly get an insurance included in the price. Otherwise you will have to purchase an insurance on your own. Make sure to read all the specifications: some situations you will be exposed to in Kenya might be out of coverage for being considered "dangerous practices".
You may like to know about the Flying Doctors Service for tourists operated by the African Medical Research Foundation (AMREF). The insurance they provide is inexpensive (USD 16 per person per month) and will cover your aeromedical evacuation to a hospital in case of emergency.
Water
Drink only bottled water and do not swim in fresh water unless you know what you're doing
In general, tap water is not drinkable in Kenya except in Nairobi and Mombasa. The Nairobi City Water and Sewerage Company (NCWSC) firmly states that "NCWSC water is safe for consumption". Yet many tourists prefer to stick to bottled water, which is the only choice outside the two big cities.
If bottled water is not available, or if you wish to cut your travel expenses (mineral water can be priced like a luxury good in Kenya), the safest method for purification is vigorous boiling for 1 minute (3 minutes at altitudes greater than 2,000 m or 6,562 feet) and cooling at room temperature. Chemical disinfection with iodine or chlorine has been traditionally used by travellers, however it is now deemed as unsafe by WHO, CDC, NaTHNaC and the European Union unless combined with other procedures such as microfiltering, since some parasites like 'Cryptosporidium' and 'Giardia' are resistant to these chemicals.
Water provided for consumption at the lodges, including ice, is perfectly safe.
 Always refrain from swimming in fresh water unless you are absolutely sure that it is safe. Waterborne parasites can penetrate through the skin, like the schistosoma (also known as bilharzia or blood-flukes, pictured at left), a flatworm that uses a freshwater snail as an intermediate host and causes schistosomiasis or bilharziosis, the world's second most devastating parasitic disease only next to malaria, according to the CDC.
Always refrain from swimming in fresh water unless you are absolutely sure that it is safe. Waterborne parasites can penetrate through the skin, like the schistosoma (also known as bilharzia or blood-flukes, pictured at left), a flatworm that uses a freshwater snail as an intermediate host and causes schistosomiasis or bilharziosis, the world's second most devastating parasitic disease only next to malaria, according to the CDC.
Schistosoma is reported by Kenya's Centre for Tropical and Travel Medicine to be prevalent at the Lake Victoria Basin as well as in the Eastern Province and the
inland coastal strip. Do not trust on crystal-clear waters, and do not swim even if locals do. The same applies to walking on mud barefooted or with open shoes. Swimming pools at the lodges are safe.
Needless to say, swimming in the sea at Kenya's coast is perfectly safe, as long as you observe the precautionary measures you would take elsewhere.
Food
Deep cooking is essential // Raw produce must be washed in clean water and peeled
 As a general rule, all food and drinks supplied at the lodges, tented camps, good hotels and international-class restaurants are presumed to be safe and clean.
As a general rule, all food and drinks supplied at the lodges, tented camps, good hotels and international-class restaurants are presumed to be safe and clean.
Away from such places, always avoid raw food such as salads, uncooked vegetables, undercooked meat or fish, juices and unpasteurised dairy products.
Remember that only deep cooking or boiling eliminates all bugs efficiently; freezing may kill protozoans, but not bacteria or viruses. Thus ice creams should only be eaten from reliable places, and do not ask for ice in your drink unless you are sure it's safe.
Fruit from unreliable sources, such as street or road vendors, can be consumed after thorough washing in safe water and/or peeling. Beware of cooked food from street vendors that has been kept at ambient temperature for a long time, since it may have been contaminated by flies.
First-aid kit
Kenyalogy's checklist will help you pack your medicines
In addition to malaria tabs and bug repellents, your first-aid kit should include a thermometer, some antiseptics (Betadine™, hydrogen peroxide and/or alcohol), an antibiotic such as Augmentin™, a paracetamol-based analgesic, ibuprofen, aspirin, an antacid, an antidiarrheal, saline solution, a cream for burns and an insect bite remedy such as After Bite™, plus cure materials like bandages, plaster, gauze and cotton.
Some anti-blister plasters (Compeed™) may come handy if you will be walking long treks. Add some pills for motion sickness if you are prone, plus your specific personal medications.
You can use Kenyalogy's Safari Packing Checklist as a guide for preparing your travel first-aid kit.
Hospitals
Nairobi has good medical care facilities
 If despite all your precautions you happen to need medical care, don't panic. In Nairobi there are some world-class facilities and medical services.
If despite all your precautions you happen to need medical care, don't panic. In Nairobi there are some world-class facilities and medical services.
The Nairobi Hospital (pictured at left) is reputed to be among the best in the whole Africa. Also outstanding are The Karen Hospital and the Aga Khan University Hospital. The latter belongs to a not-for-profit international organisation that also hosts another Aga Khan Hospital in Mombasa. Nairobi Women's Hospital, with four branches, is specialised in obstetrics and gynecology but cares for all health matters of women and children.
The country's main reference public hospital is Kenyatta National Hospital, the largest and oldest in Kenya, which hosts the University of Nairobi Medical School.
Nevertheless and other than the aforementioned, the real picture of Kenya's health care system is downright devastating. In the rest of the country there are only modest clinics, and even public hospitals in the cities are frequently understaffed and poorly equipped.
|



